|
Getting your Trinity Audio player ready...
|
Understanding the Medication Challenge
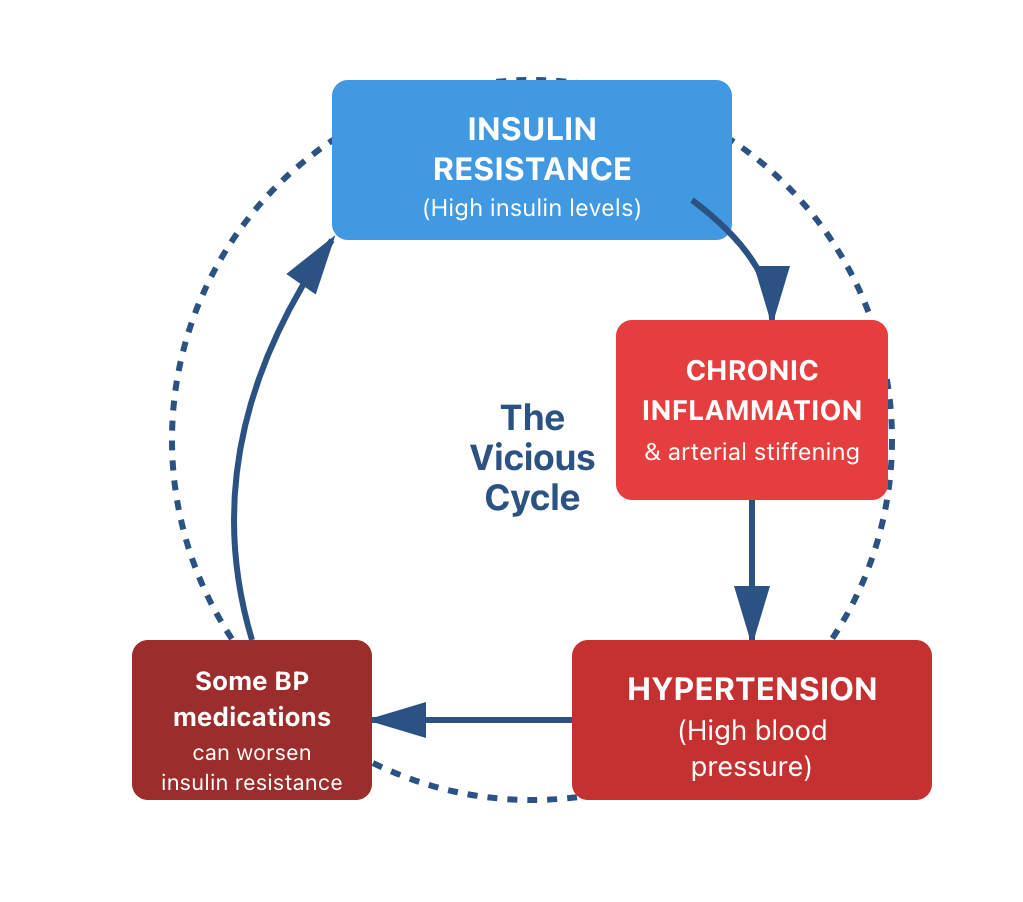
Your blood pressure medication may be controlling your numbers—but research shows that some of the most commonly prescribed drugs may be worsening the underlying metabolic condition that contributes to hypertension in the first place. This isn’t about blaming doctors or medications. It’s about understanding that while blood pressure control is important, addressing the root cause offers a path to genuine health restoration. Research demonstrates an important paradox: certain widely-used antihypertensive medications can reduce blood pressure readings while simultaneously worsening insulin resistance—a key metabolic factor that contributes to hypertension.Key Findings:
- 60-70% of hypertension patients take medications that may worsen insulin resistance
- Low-carb diet + fasting: reduces insulin resistance & arterial stiffening without drugs)
- Insulin resistance develops 5-20 years before hypertension diagnosis
- It’s completely reversible with dietary intervention
Dr. Pradip Jamnadas, MD
In his lecture “Treat High Blood Pressure’s Root Cause” (July 13, 2021), Dr. Jamnadas explains the connection between insulin resistance and arterial changes:“The most common reason for hypertension is metabolic syndrome—insulin resistance. High insulin causes the kidneys to retain salt, which increases blood volume. But more importantly, insulin is a growth factor. It causes the smooth muscle cells in your artery walls to grow, making the arteries stiff and narrow. This inflammation and stiffening is what leads to high blood pressure.”
Dr. William Davis, MD
From his blog post “Reverse INSULIN RESISTANCE” (November 21, 2020):“Insulin resistance leads to cognitive impairment/dementia, coronary disease, fatty liver, hypertension and cancer.” “Visceral fat surrounding abdominal organs and heart is a huge driver of hypertension, cultivated by insulin resistance resulting from grain and sugar consumption.”
Source: His blog “The Pharmaceuticalisation of Americans: Blood Pressure” Date: November 14, 2017
The Time Gap That Hides the Connection
Because insulin resistance typically develops years or even decades before diagnosable disease emerges, the connection between cause and effect often goes unrecognised. For example:- Obsessive-compulsive disorder (OCD) may manifest in childhood—the same time insulin resistance can begin developing
- Individuals with larger body frames who experience persistent low mood or depression may be responding to underlying insulin resistance, yet only develop clinically diagnosed hypertension years or decades later
Signs of Insulin Resistance
Common conditions linked to insulin resistance can vary between men and women:For men:
- Depression or persistent low mood
- Brain fog and cognitive difficulties
- Lack of motivation or drive
- Reduced stress resilience
- Poor sleep quality
- Increased fatigue
- Chronic low-grade inflammation
- Increased visceral (abdominal) fat
For Women:
- Irregular, unpredictable, or absent menstrual cycles
- Persistent hunger, even shortly after eating
- Brain fog and mental cloudiness
- Depression or persistent low mood
- Increased fatigue
- Chronic low-grade inflammation
- Increased visceral fat
 The Root Cause Solution
The Root Cause Solution
Low-Carbohydrate Diet and Intermittent Fasting
A very low-carbohydrate diet combined with intermittent fasting directly addresses the root cause by lowering insulin levels and reversing insulin resistance.
The Research:
A systematic review found that low-carbohydrate diets produced significant reductions in blood pressure. BMJ Case Report: Ketogenic diet plus intermittent fasting reversed type 2 diabetes in 4 months, while eliminating hypertension medications within weeks—demonstrating rapid metabolic restoration addressing both conditions simultaneously.
Most importantly: These improvements occurred while improving metabolic health—the opposite of what happens with some medications that lower blood pressure while worsening insulin resistance. Here are studies that show hypertension and other diseases directly linked to insulin resistance.
How It Works:
- Reduced carbohydrate intake lowers insulin secretion
- Intermittent fasting enhances insulin sensitivity & cleans the cells through autophagy
- Together they reduce visceral fat—directly reversing the insulin resistance that contributes to arterial stiffening and hypertension
The Supporting Evidence
Study 1: Hydrochlorothiazide and Insulin Resistance
Title: Hydrochlorothiazide, but not Candesartan, Aggravates Insulin Resistance and Causes Visceral and Hepatic Fat Accumulation
Date: December 2008
Finding: After only 12 weeks of hydrochlorothiazide treatment in abdominally obese hypertensive patients, researchers found worsened insulin resistance, visceral fat redistribution, and increased liver fat accumulation with elevated liver enzymes. Candesartan (an ARB) showed no such metabolic effects.
View the study
Study 2: Beta-Blockers and Long-Term Metabolic Effects
Title: Long-term metabolic effects of antihypertensive drugs
Date: 1994
Finding: Using the gold-standard hyperinsulinemic euglycemic clamp method, this study found that treatment with beta-blockers named: pindolol, propranolol, metoprolol, atenolol and hydrochlorothiazide caused significant decreases in insulin sensitivity after 4-6 months that persisted unchanged after 2-3 years of treatment. ACE inhibitor captopril increased insulin sensitivity without affecting serum lipids.
View the study
Study 3: Low-Carbohydrate Diet Benefits
Title: Effects of low-carbohydrate and low-fat diets: a randomised trial
Date: September 2014 (Annals of Internal Medicine)
Finding: A low-carbohydrate diet produced greater reductions in blood pressure compared to a low-fat diet, with participants experiencing significant decreases in both systolic and diastolic blood pressure. The low-carbohydrate group also showed greater improvements in insulin sensitivity and metabolic markers.
View the study
Ready to Address the Root Cause?
You have three options to start your journey to genuine health restoration:
Option 1: Test Your Insulin Resistance Level
The NHS doesn’t test for insulin resistance. A simple £149 HOMA-IR test could detect it while it’s still has no significantly negative health effects.